SHOP PRODUCTS
Logitech provides award-winning, beautifully designed peripherals for everyone at work, home, and school. Improve performance, comfort, and style while decluttering your desk, home, and office.
MICE + KEYBOARDS
Precision, comfort, and expression: Shop wired and wireless mice and keyboards. Choose from products with Bluetooth®, that are built for performance, ergonomics, travel, home office, and more.


Shop wireless and wired mice. Choose from Bluetooth, performance, ergonomic, business, EDU, travel, compact, and WFH products.


Shop keyboard and mouse combos. Choose from ergonomic, essentials, compact, performance, wireless, Bluetooth, and portable products.
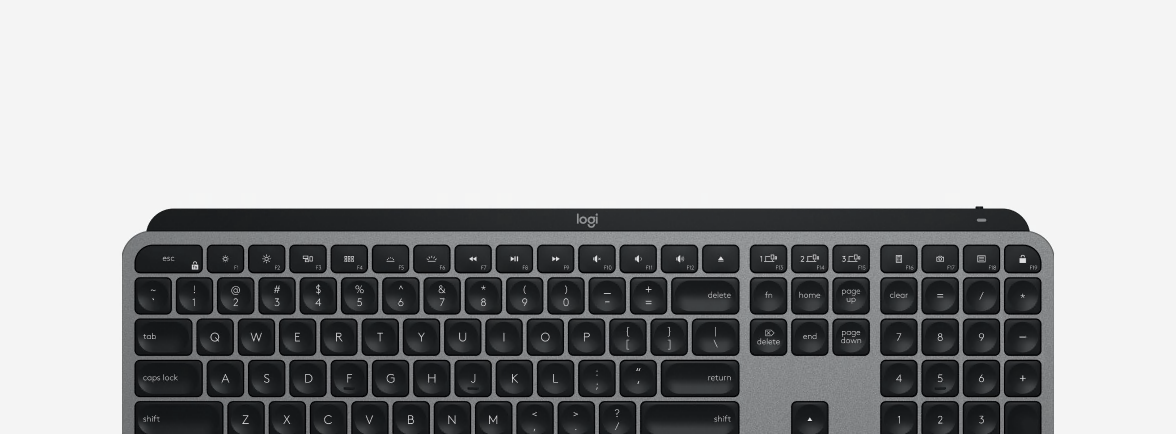
Shop wired and wireless keyboards. Choose from mechanical, ergonomic, comfort, portable, Bluetooth, multi-device, and multi-OS products.


Shop Tablet Keyboards and Cases. Universal Bluetooth wireless keyboards and cases for select Android™, Apple, Samsung®, Amazon™, and Windows® tablets.


Shop wireless and wired mice. Choose from Bluetooth, performance, ergonomic, business, EDU, travel, compact, and WFH products.


Shop keyboard and mouse combos. Choose from ergonomic, essentials, compact, performance, wireless, Bluetooth, and portable products.
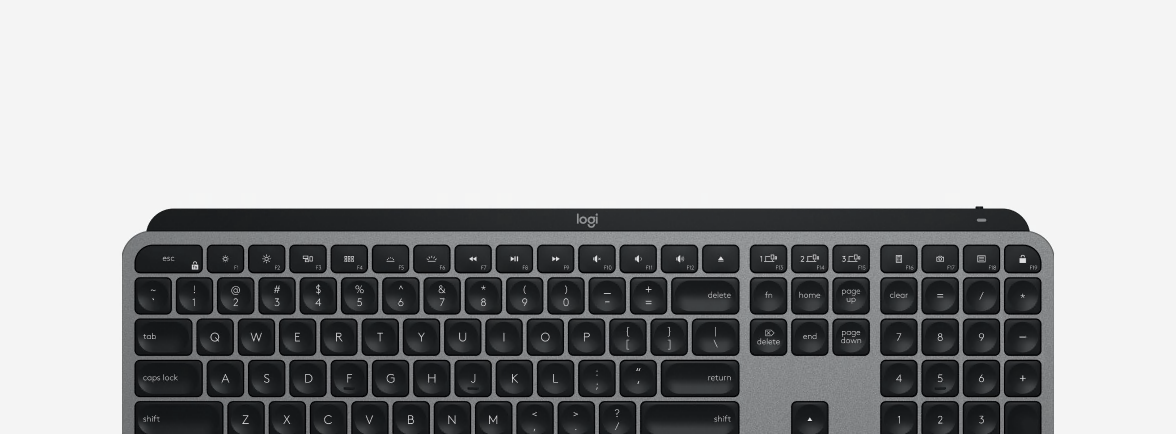
Shop wired and wireless keyboards. Choose from mechanical, ergonomic, comfort, portable, Bluetooth, multi-device, and multi-OS products.


Shop Tablet Keyboards and Cases. Universal Bluetooth wireless keyboards and cases for select Android™, Apple, Samsung®, Amazon™, and Windows® tablets.
HEADSETS + SPEAKERS
Shop wired and wireless headsets and speakers with high-quality sound. Choose from products featuring noise cancellation, Bluetooth USB connections, long battery life, and more.


Shop wired headsets. Choose from products with USB or 3.5 mm connections. Works with popular conferencing apps.


Shop Bluetooth speakers including 5.1 surround sound systems, stereo computer speakers, and 2.1 systems with a subwoofer.


Shop wireless headsets. Choose from products featuring Bluetooth or USB connections, ANC, noise cancellation, and more.


Shop computer speakers for bookshelves, stereos, and desktops and full systems with subwoofers.


Shop headset and webcam bundle kits. Choose from a wireless headset and a 4K webcam or a wired headset with a 1080p webcam.


Shop surround systems including 5.1 speaker systems with Bluetooth or a THX, Dolby Digital, and DTS certified systems.


Shop wired headsets. Choose from products with USB or 3.5 mm connections. Works with popular conferencing apps.


Shop Bluetooth speakers including 5.1 surround sound systems, stereo computer speakers, and 2.1 systems with a subwoofer.


Shop wireless headsets. Choose from products featuring Bluetooth or USB connections, ANC, noise cancellation, and more.


Shop computer speakers for bookshelves, stereos, and desktops and full systems with subwoofers.


Shop headset and webcam bundle kits. Choose from a wireless headset and a 4K webcam or a wired headset with a 1080p webcam.


Shop surround systems including 5.1 speaker systems with Bluetooth or a THX, Dolby Digital, and DTS certified systems.
STREAMING
From first stream to mainstream, shop streaming products that give you a professional edge on Twitch or YouTube, whether you’re new or established in your career. Find webcams, green screens, microphones, and more.


Shop webcams for video conferencing, business, education, and working from home. High quality webcams with crystal clear 4K, 1080p, or 720p.


Shop the portable green screen you can unfold in seconds. Instantly give a professional edge to business meetings, remote lessons, streams, and content creation.


We make tools, you change the world. Make a scene, raise your voice, and take control with Logitech for Creators.


Shop webcams for video conferencing, business, education, and working from home. High quality webcams with crystal clear 4K, 1080p, or 720p.


Shop the portable green screen you can unfold in seconds. Instantly give a professional edge to business meetings, remote lessons, streams, and content creation.


We make tools, you change the world. Make a scene, raise your voice, and take control with Logitech for Creators.
VIDEO CONFERENCING
Collaborate in virtual meetings, in-office, and distance learning. Shop video conferencing products like webcams and accessories for desk and mobile setups, conference rooms, and more.


Shop webcams designed to work with any VC software for video conferencing, business, education, and working from home. High quality webcams with crystal clear 4K, 1080p, or 720p.


Add features and flexibility with these video conferencing accessories that include cabling, speakers, mics, mounts, and replacement parts.


Browse conference room cameras. Choose from all-in-one video bar, video conferencing camera systems, and portable cameras with speakerphones.


Browse room solutions. Easy to use, high quality conferencing solutions for all room sizes. Compatible with software platforms like Zoom®, Google®, and Microsoft®.


Logitech enables the same seamless audio and video experience from any workspace - office, home, or hot desk.


Shop webcams designed to work with any VC software for video conferencing, business, education, and working from home. High quality webcams with crystal clear 4K, 1080p, or 720p.


Add features and flexibility with these video conferencing accessories that include cabling, speakers, mics, mounts, and replacement parts.


Browse conference room cameras. Choose from all-in-one video bar, video conferencing camera systems, and portable cameras with speakerphones.


Browse room solutions. Easy to use, high quality conferencing solutions for all room sizes. Compatible with software platforms like Zoom®, Google®, and Microsoft®.


Logitech enables the same seamless audio and video experience from any workspace - office, home, or hot desk.
MOBILE DEVICES
Mobile device accessories for your mobile lifestyle. Shop iPad, Tablet, and Smartphone keyboards, accessories, and more.


Shop keyboards for iPad®, iPad® Air, and iPad® Pro. Unlock potential with Logitech keyboards designed to help you work, learn, and enjoy more.


Shop tablet keyboards and cases. Improve usability with universal Bluetooth wireless keyboards and cases for select Android, Apple, Samsung, Amazon, and Windows tablets.


Shop iPad Accessories. Make your tablet better and easier to use with wireless mice, charging stands, and digital pencils.


Shop smartphone accessories. Choose from multi-device Bluetooth keyboards, cell phone charging stands, wireless chargers, and more.


Shop keyboards for iPad®, iPad® Air, and iPad® Pro. Unlock potential with Logitech keyboards designed to help you work, learn, and enjoy more.


Shop tablet keyboards and cases. Improve usability with universal Bluetooth wireless keyboards and cases for select Android, Apple, Samsung, Amazon, and Windows tablets.


Shop iPad Accessories. Make your tablet better and easier to use with wireless mice, charging stands, and digital pencils.


Shop smartphone accessories. Choose from multi-device Bluetooth keyboards, cell phone charging stands, wireless chargers, and more.
HOME SECURITY
Build a smart home and stay secure. Shop accessories and video doorbells, that work with the ever-growing constellation of smart devices.


Shop the Apple HomeKit-enabled security camera with best-in-class Logitech TrueView video.


Shop the Apple HomeKit-enabled video doorbell with Face Recognition for Logitech.


Shop the Apple HomeKit-enabled security camera with best-in-class Logitech TrueView video.


Shop the Apple HomeKit-enabled video doorbell with Face Recognition for Logitech.
LOGITECH SOLUTIONS
From coding and creating to comfort, shop Logitech’s solutions for professionals. Find mice, keyboards, accessories, and more designed with you in mind.


Unleash your capability to create, make, and do. Shop MX products to master your next project with tools that transform the way you work.


Bring wellness into your workplace. Shop ergonomic products that improve posture, effectiveness, and comfort.


Unleash your capability to create, make, and do. Shop MX products to master your next project with tools that transform the way you work.


Bring wellness into your workplace. Shop ergonomic products that improve posture, effectiveness, and comfort.